As early as 1984, U.S. Secretary of Health Margaret Heckler declared that a vaccine would be available within two years. A vision shared by others - the virus had only just been discovered and the complexity of its pathophysiology was then very far from being fully appreciated. Moreover, the development in the 1970s and 1980s of vaccines based on viral or bacterial proteins, rather than just whole microorganisms, reinforced this optimism.
But the efforts of researchers and doctors were going to face many difficulties for many years to come. So much so that, 34 years later, the development of a prophylactic vaccine remains a priority in HIV research. Today, however, the end of the tunnel seems closer than ever.
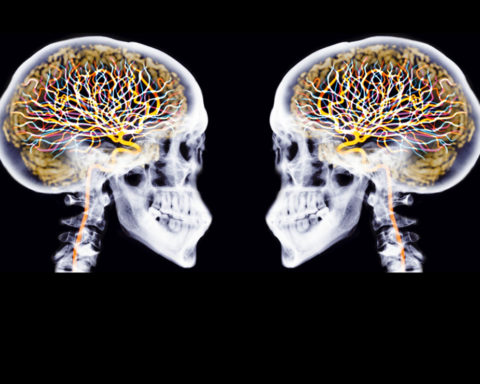
Lymphocytes, major players in immunity
Our body has three lines of defence against pathogenic micro-organisms, especially viruses. The first is the barrier of the skin and mucous membranes. If this barrier is breached, the invader faces innate immunity, which is based on cells capable of recognizing foreign agents. To do this, they detect components present on their surface (sugars, proteins...), called antigens. This immunity is not specific to a particular agent, it attacks everything that is not the organism. It also prepares the third line of defence, acquired immunity. It is the latter that is stimulated by vaccination.
Acquired immunity is more subtle than innate immunity, and most importantly, it is specific: its agents are capable of recognizing and attacking a particular microorganism. It also retains the memory of previous encounters, which generally allows it to react more quickly in the event of a new invasion by the same pathogen.
Acquired immunity is complex, but its essential actors are a particular class of white blood cells, the lymphocytes. There are several types of white blood cells, including B lymphocytes (LB) and CD8+ T lymphocytes (CD8 LT), which play a major role. The former produce antibodies, molecules capable of specifically binding to an invader to coat and neutralize it. Another role of antibodies is to attract the attention of immune system cells that will destroy the coated viruses. CD8 LTs, on the other hand, directly destroy the cells infected by the viruses, thus preventing the spread of the infection.
The action of these two categories of lymphocytes is coordinated by a third type of lymphocyte, the CD4+ LT lymphocytes (CD4 LT), which stimulates them, acting in a way as conductors of the acquired immune response. These CD4+ T lymphocytes are the main target of HIV, which destroys them, making it very difficult to mount an effective immune response.
How does acquired immunity work?
Train the organization to defend itself
Vaccination is to the immune response what major maneuvers are to military training. It simulates an infection by making the organism believe that an invader has crossed its lines, in order to trigger its immune response. This way, when the organism actually encounters the affected microbe, it will react more quickly.
The vaccines used may contain either fragments of the microbe(s) against which protection is desired (protein vaccines), whole killed microbes (inactivated vaccines), or live but attenuated, non-virulent forms of these microbes (live attenuated vaccines).
Live attenuated vaccines are those that induce immune protection closest to that resulting from natural infection, resulting in both antibody production and stimulation of CD8 LT. However, their use carries a low risk of inducing vaccine-borne infectious disease if the micro-organisms they contain regain their virulence. For obvious safety reasons, this type of vaccine could not be used in the case of HIV.
Subterfuges had to be used to achieve the same type of optimal immune response. But several obstacles stood in the way.
HIV, an elusive virus
One of the main problems that scientists working on HIV vaccine development have faced is the extreme viral diversity. There are two main types of HIV viruses: HIV1 and HIV2, classified into various groups according to their origin (each group can be further subdivided into subtypes).
HIV2 (divided into nine groups, from A to I) is mainly found in patients from West Africa, and to a very small extent in people from Western countries and India (in France it accounts for 1 to 2 % of infections). HIV1 can be subdivided into four groups: M (Major, responsible for the majority of HIV1 infections), O (Outlier), N (non-M, non-O), P (last identified, in 2009).
The HIV genome does not consist of DNA, but of RNA. Like all RNA viruses, it makes a lot of mistakes as it multiplies. It gives rise to many variants that differ slightly from each other. This leads to a very high viral diversity not only between infected people, but also within each infected person. A single infected patient can be a carrier of million different variantsThis is more than the diversity generated during a global flu epidemic! The latter requires the development of an new vaccine every year…
The second major problem with developing a vaccine is that HIV infection does not necessarily lead to protection. This is because the antibodies produced after HIV infection do not provide sufficient protection. Furthermore, CD8 LTs are able to control the replication of the virus, but not to suppress the infection. Finally, the "natural" immunity that could be obtained does not prevent superinfections by other strains of HIV .
In the absence of treatment, HIV-infected patients will therefore inevitably end up progressing towards the stage of AIDSwith the notable exception of a small specific group of patients called elite controllers. The latter, which represent less than 1 % of the infected population, possess CD8 TLs capable of destroying infected CD4 TLs, and thus containing the infection.
First milestones in vaccine research
As early as 1987, a French team tested a live attenuated vaccine containing a modified vaccinia virus to get him to make an HIV-1 protein. It was known that this then new technology could induce antibody synthesis and stimulate CD8 LT. Unfortunately, the trials were inconclusive.
Almost all available vaccines against other infections rely on the induction of neutralizing antibodies, which block the pathogen from entering the patient's cells. Early HIV vaccine strategies therefore targeted the induction of such antibodies. However, in the case of HIV, these neutralizing antibodies are only effective against a few strains of the virus. They cannot neutralize the plethora of variants present in a patient's body.
The first phase 3 clinical trials (trials to evaluate the effectiveness of a drug) of HIV vaccines that are supposed to produce neutralizing antibodies took place from 1998 to 2002. Called AIDSVAX, they involved more than 7,000 participants in North America, the Netherlands, and Thailand.
Inspired by the efficacy of the hepatitis B vaccine, which is based solely on the proteins present on the virus envelope, these HIV vaccines were protein vaccines containing an HIV envelope protein (from two HIV subtypes1 common in the geographic areas where the trials were conducted). But these trials failed to protect against infection.
A year later, another Phase 3 trial entitled RV144 started in Thailand. Conducted from 2003 to 2009, and involving more than 16,400 participants, it took the HIV protein used in AIDSVAX and combined it with a harmless viral vector, the canarypox virus, which produces other HIV proteins.
For the first time, this approach provided partial protection against HIV infection. Results released in 2009 showed that the vaccine protected 31.2 % of participants.
The most promising current strategies
While the results of the RV144 trial were encouraging, they raised three issues:
-
they were based on a single test and the protection provided was of short duration;
-
the protection was a priori directed only against the only virus subtype;
-
This type of strategy did not induce broad-spectrum neutralizing antibodies capable of blocking all existing types of HIV.
To find an answer to the first point, the HVTN702 trial was set up in South Africa. It is based on the same strategy as the RV144 trial, but the vaccines are produced from a strain of HIV that is predominant in Africa and the trial involves an additional injection of vaccine one year after the initial injection to increase the duration of the immune response. The trial is scheduled to begin in November 2017, its results are expected in January 2022.
In an attempt to address the second problem, the lack of diversity in protection, researchers have developed mosaic" vaccines. The vaccination strategy remains broadly the same. It uses two different vaccines, a viral vector and envelope proteins. However, the viral vector no longer produces a whole protein from a single strain of HIV, but pieces of protein from several strains. These have been identified by researchers using bioinformatics as capable of inducing a broader immune response.
This strategy, validated in non-human primate models, again led to the establishment of an efficacy trial. Called HVTN 705/HPX2008 " Imbokodo "It began in November 2018. It is expected to include 2,600 women in five countries in sub-Saharan Africa (mainly South Africa), and is scheduled to end in 2022.
Both strategies are likely to result in success rates of around 50 %. This may seem low, but having an effective vaccine at 50 % would be a great step forward, not only at the individual level but also at the population level. The vaccinated populations would be those living in areas of high virus endemicity or at risk (MSM...prostitutes...). The impact of such a vaccine on the evolution of the epidemic has been very well modelled, in particular by the International AIDS Vaccine Initiative (IAVI) consortium.
The grail of neutralizing antibodies
Important as these advances are, they do not induce broad-spectrum neutralizing antibodies. This is the only way to ensure highly efficient protection at the individual level.
While it has long been thought that such a vaccine would remain a pipe dream, recent data suggest that this is not the case. Studies conducted in the United States in cohorts of at-risk individuals have shown that broad-spectrum neutralizing antibodies can be detected in approximately 1 % of HIV-infected individuals.
Despite the presence of these antibodies, however, the virus continues to replicate in patients' bodies. However, when these neutralizing antibodies are purified, they are able to block the infection by more than 90 to 95 % of HIV1 strains...in a laboratory.
This is an important finding. If, in the long run, an individual infected with HIV has to defend himself or herself against many different viruses, he or she is initially infected with only one virus. If a vaccine could induce such neutralizing antibodies, it would therefore be protective at 90 to 95 %!
Strategies to induce such antibodies are being tested in animal trials. They are quite complex, and their clinical development in humans is much less advanced than those previously described.
Other HIV vaccine strategies have been developed, based in particular on induction of a CD8 LT response. Unfortunately, most of them have proved ineffective. in human clinical trials.
With regard to CD8 LT, only one track seems promising, but it has been evaluated only in non-human primates, and induces a protection of 50 %.
The search for an HIV vaccine therefore remains very active and the results of the two ongoing phase 3 clinical trials are eagerly awaited. In addition, the recent discovery of the existence of broad-spectrum neutralizing antibodies in some patients represents great hope for the future development of an effective vaccine at the individual level.
And whatever the results, the knowledge gained from this HIV-related work will help improve the design of vaccines against other complex and highly mutable pathogens, such as influenza.
Jean-Daniel LelièvrePU-PH head of department - director of the clinical department of the VRI, National Institute of Health and Medical Research (Inserm)
This article is republished from The ConversationUP' Magazine's editorial partner. Read theoriginal paper.
Anything to add? Say it as a comment.![]()